Know your Medicaid revenue cycle KPIs
How will potential changes in Medicaid spending impact your revenue cycle? Now is the time to know.
Apr 21, 2025
Apr 21, 2025

We read the healthcare business news as much as you do. As a healthcare revenue cycle leader, you no doubt have seen headlines like these over the past month:
- “75% of this hospital’s patients are on Medicaid. Here’s how it’s bracing for potential cuts.”—Becker’s Hospital Review
- “Hospitals one of the biggest losers from Medicaid cuts, state treasurers say.”—Healthcare Finance News
- “Providers face $80B losses without Medicaid expansion.”—Rev Cycle Management
Clearly, Medicaid spending has become a political hot potato in Washington. The challenge for revenue cycle leaders like you is preventing that hot potato from landing in your lap.
Prevention starts with preparation. This would be the perfect time to focus on your Medicaid revenue cycle key performance indicators. We track them through our Payor Market Intelligence tool. PMI is based on real data from the 2,000 hospitals and 300,000 physicians who use Kodiak Revenue Cycle Intelligence to manage their net revenue and monitor their revenue cycle performance.
One of the many reasons we watch Medicaid revenue cycle KPIs closely is that Medicaid historically has been a notorious underpayer that pays claims slowly. As one of the two largest public health insurance programs—Medicare being the other—payment shortfalls from Medicaid mean providers must make up those payment deficits from other payors, mostly commercial health plans.
Underpayments were a hot topic of conversation at Kodiak’s invitation-only Revenue Circle conference held Jan. 26-28, 2025, in Scottsdale, Arizona. Other hot topics at the event included denials management, strategic pricing, revenue integrity, and automation.
So, which Medicaid KPIs should you as a revenue cycle leader start tracking even closer to see if, when, and how what happens in Washington is affecting your organization?
We recommend at least these five:
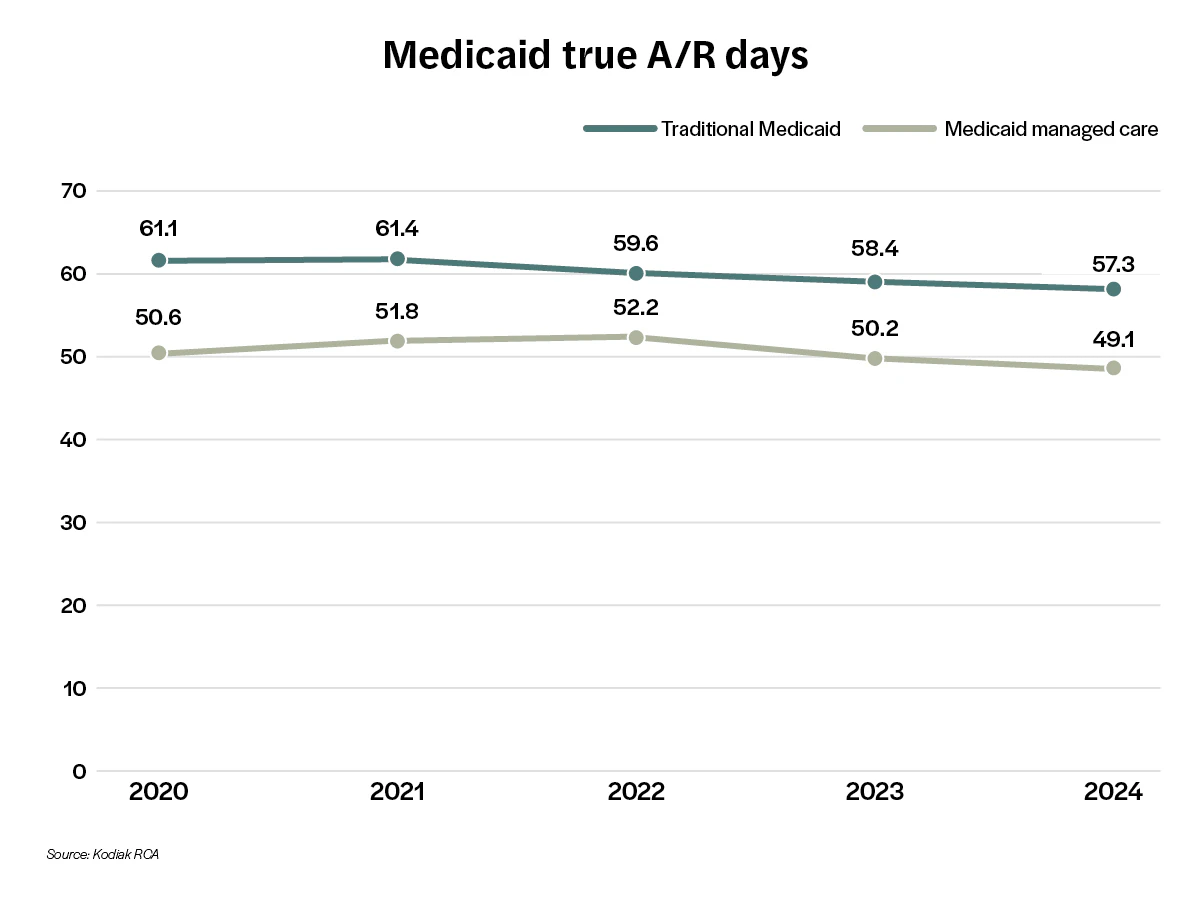
- True accounts receivable days
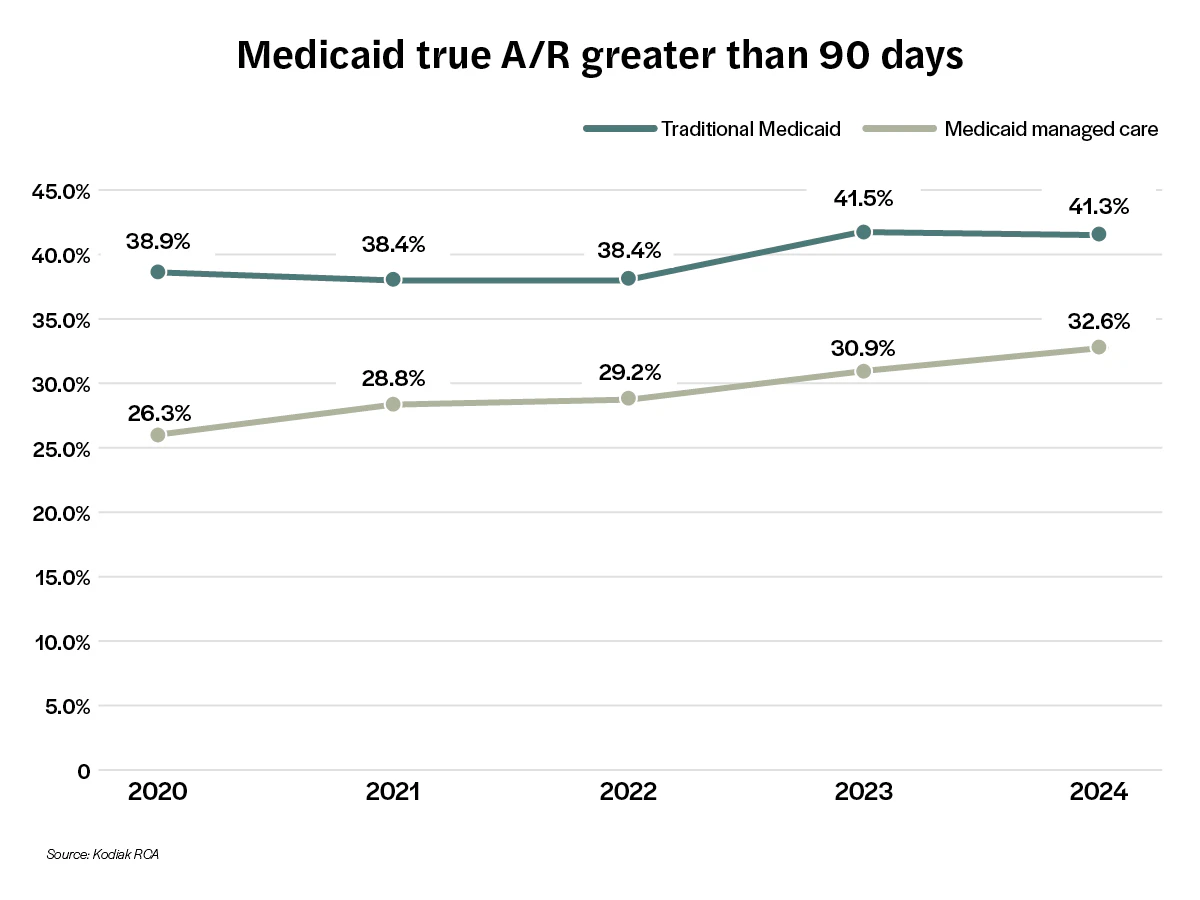
- True A/R greater than 90 days as a percentage of true A/R days
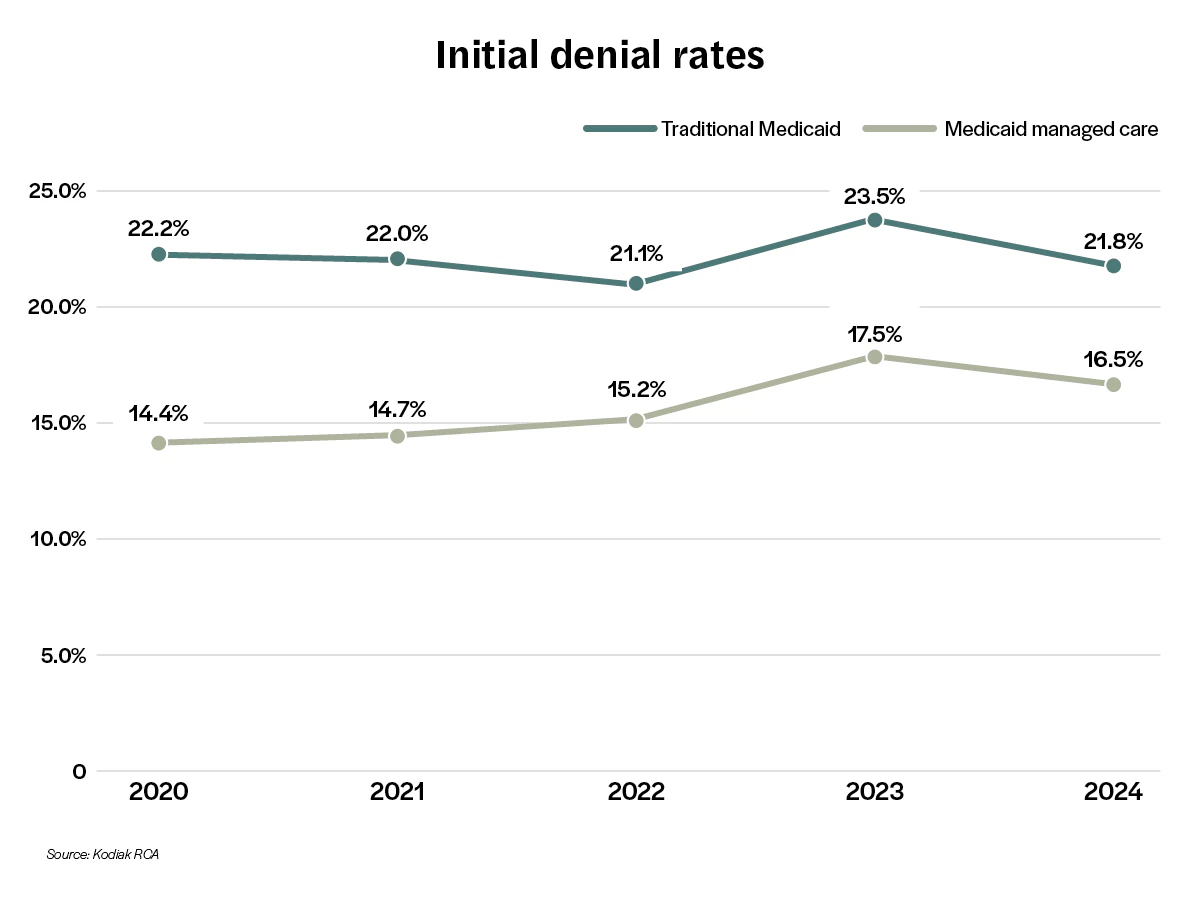
- Initial claim denial rate
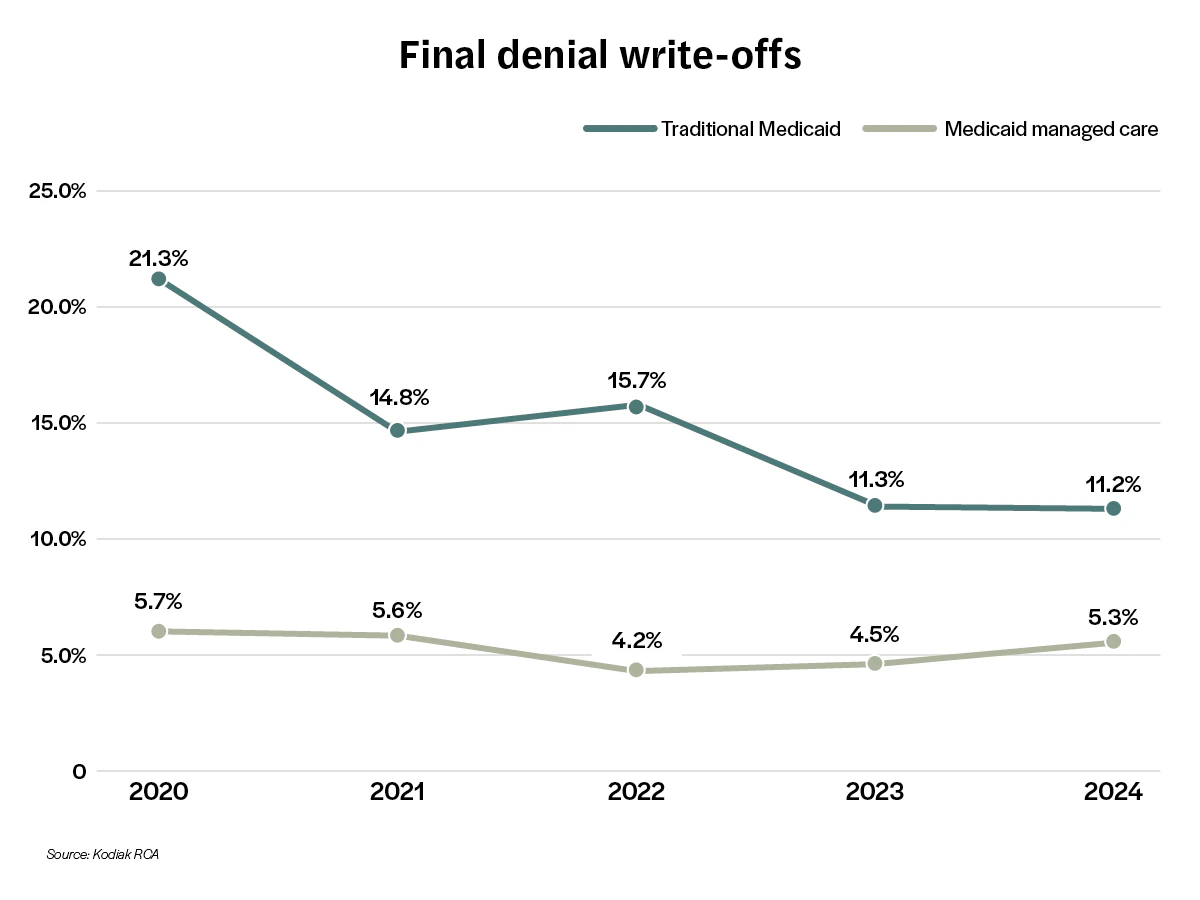
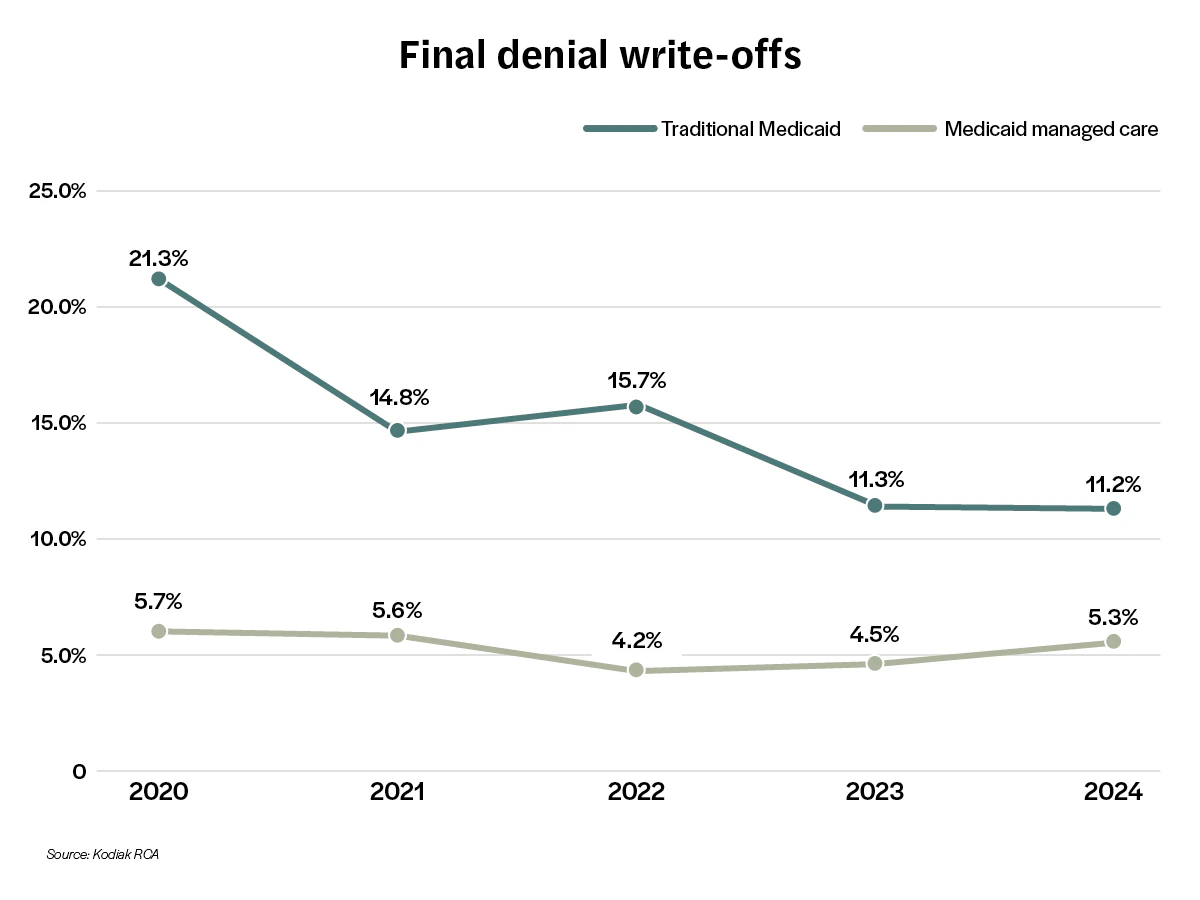
- Final denial write-off as a percentage of net Medicaid patient service revenue
- Bad debt as a percentage of gross Medicaid patient service revenue
We also recommend that you track these five revenue cycle KPIs by traditional Medicaid, or fee-for-service Medicaid, and by Medicaid managed care, or care provided to Medicaid recipients through Medicaid HMOs and other types of managed care plans.
Below are five charts that track each of the five KPIs by traditional Medicaid and Medicaid managed care over the past five years and what the trend lines suggest for each KPI.
Trend 1: Medicaid true A/R days have been declining.
Trend 2: Medicaid true A/R greater than 90 days has been rising.
Trend 3: Initial denial rates came down in 2024 after a five-year high.
Trend 4: Final denial write-offs for traditional Medicaid have dropped, while final denial write-offs for Medicaid managed care have crept up.
Trend 5: Though still less than 1% of gross Medicaid patient service revenue, bad debt also crept up in 2024.
These five trends represent a mix of good news and bad news for hospitals, health systems, and medical practices. On the positive side, A/R days and initial denial rates were down last year. On the negative side, A/R greater than 90 days and bad debt were up last year.
It’s important to remember that these aggregated national benchmarks mask the likely wide variations in Medicaid revenue cycle KPIs by states and their individual state Medicaid programs. That’s why it’s so important for you to know your state’s Medicaid KPIs and your organization’s Medicaid KPIs. You should know how you compare with your peers in your state and nationally. Only then will you know how what’s happening in Washington is impacting your revenue cycle performance.
If you need help with that, we’re here for you with PMI and our entire revenue cycle performance team.
Read more insights from the Kodiak Revenue Circle:
- “11 priorities facing healthcare revenue cycle leaders in 2025”
- “7 payor do's and don’ts from your provider peers.”
- “Cost shifting but smarter.”
Want to learn more about your Medicaid revenue cycle performance? Kodiak has you covered.
Contact Us
Want the latest updates from Kodiak?
Get access to our communications, including our Healthcare Connection newsletter, to tap into industry trends, CPE webinars, and more.



