2024 Healthcare Summit attendee poll results
2024 Kodiak Healthcare Summit attendee polls identify the top reimbursement and revenue cycle challenges facing healthcare financial leaders.
Oct 9, 2024

Taking the pulse of finance and revenue cycle leaders is a hallmark of the annual Kodiak Healthcare Summit. We did it again at this year’s Summit, held in Nashville and virtually Sept. 22-25. More than 500 of you attended Summit in person or online. You weren’t shy about telling us what’s on your mind through a series of attendee polls taken during the dozens of educational sessions at the four-day event.
Here are six interesting things on your mind that are giving us here at Kodiak Solutions more food—and fuel—for thought as we build out the technologies, tools, services, and solutions you need to excel at net revenue reporting and revenue cycle management.
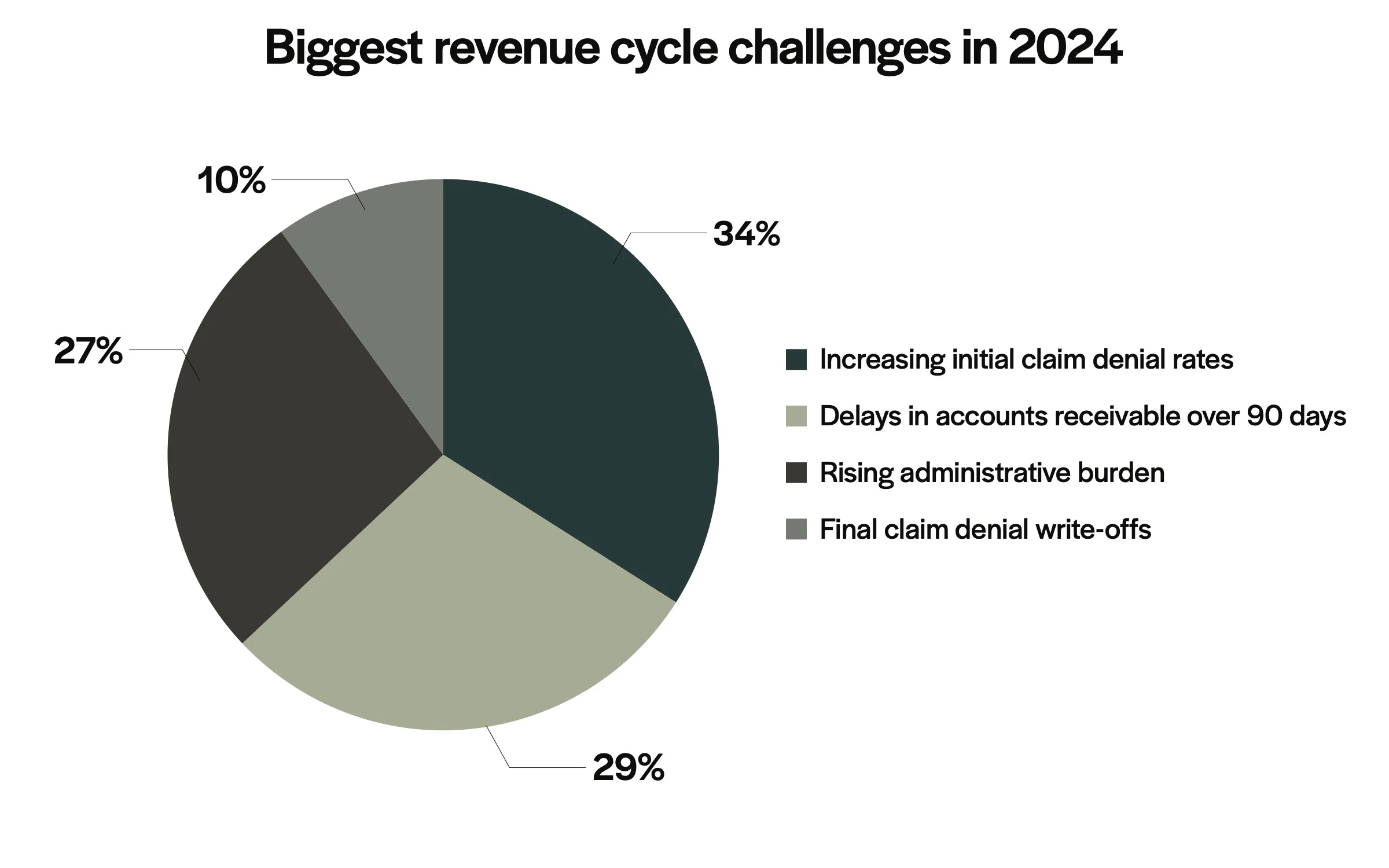
1. We asked you what you thought your biggest revenue cycle challenge was.
You said it was increasing initial claim denial rates.
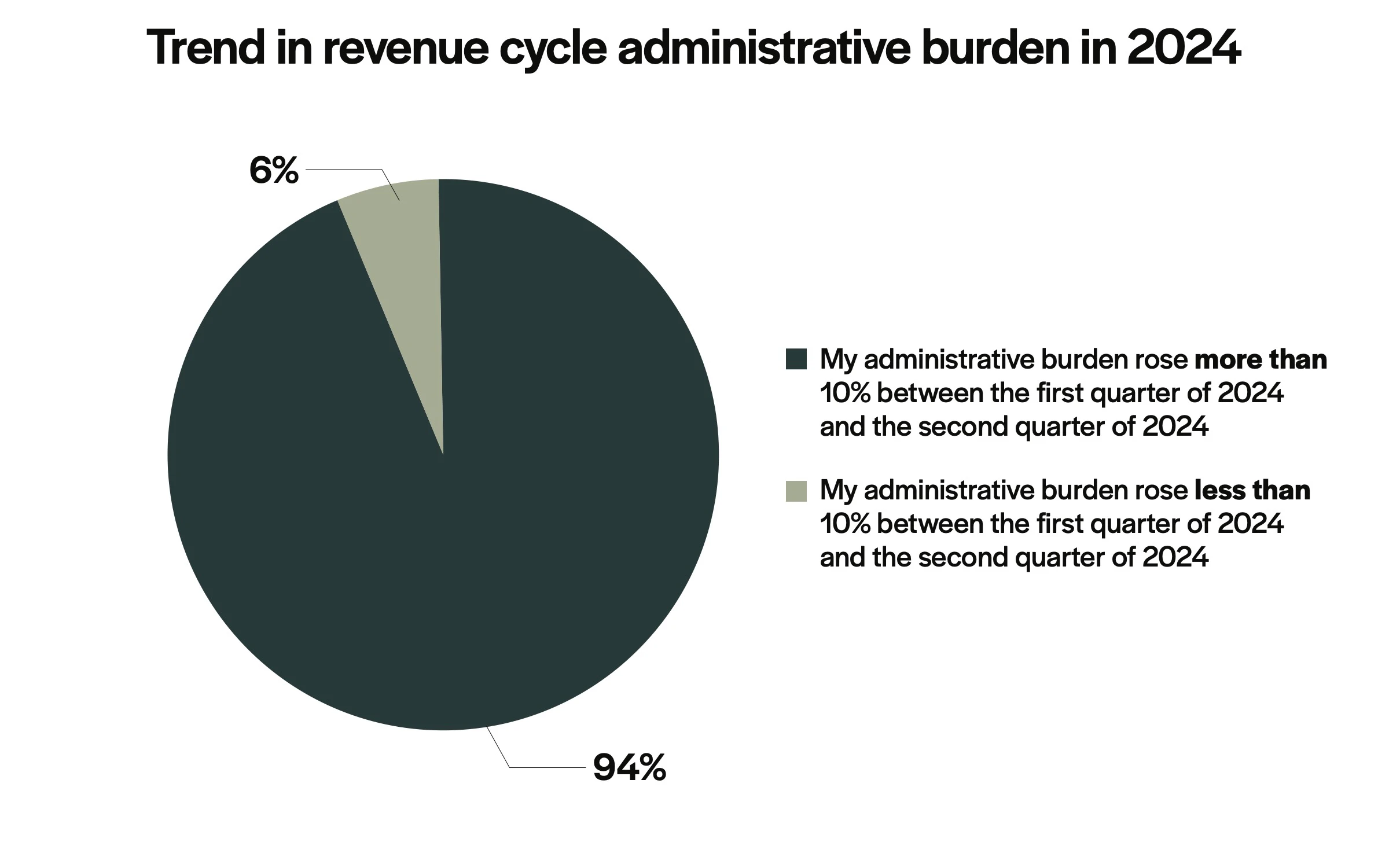
2. We asked you whether you thought your revenue cycle administrative burden was growing this year.
You said it’s jumped more than 10% this year.
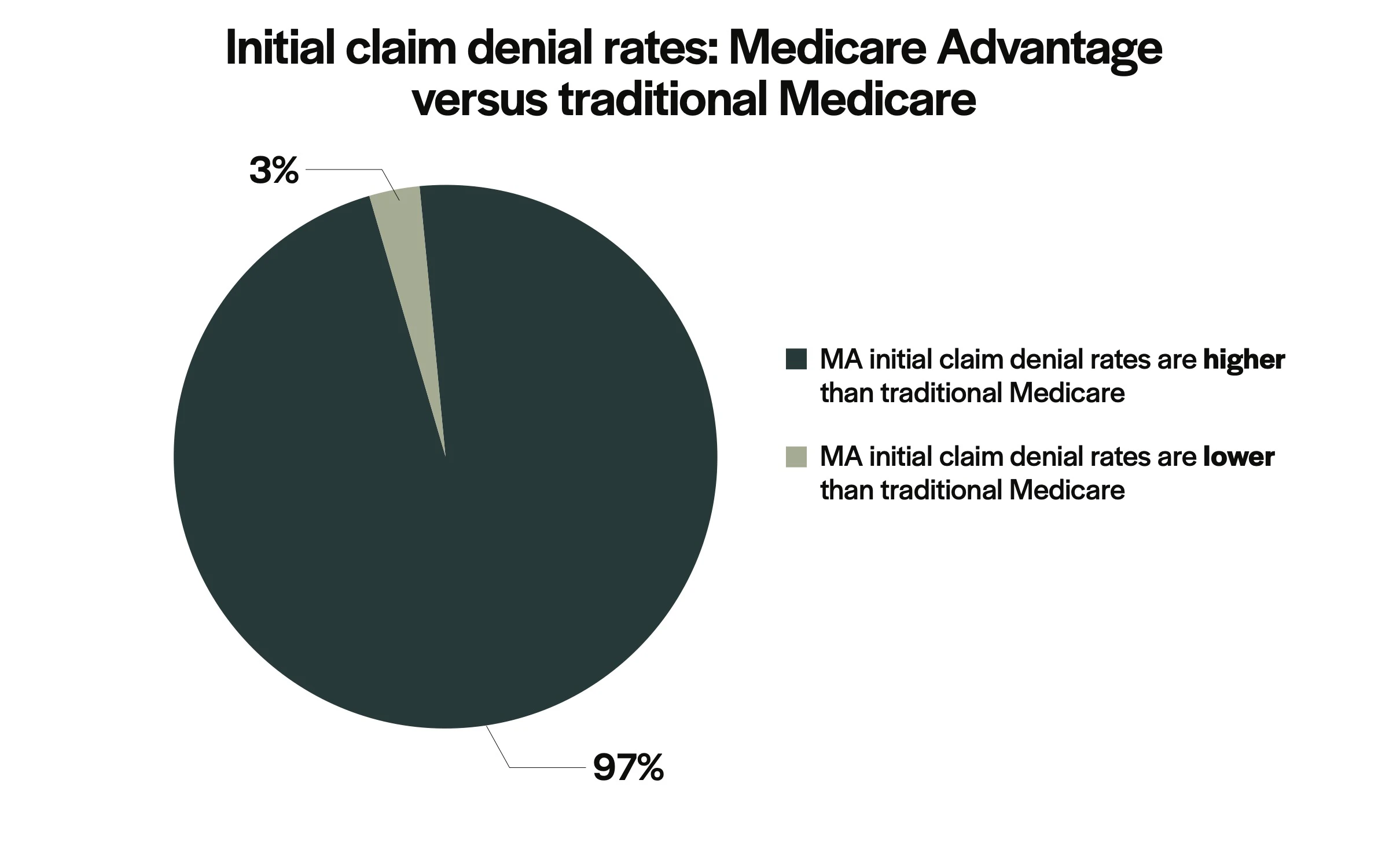
3. We asked you whether you thought Medicare Advantage plans have a higher initial claim denial rate than traditional Medicare.
You said yes, overwhelmingly.
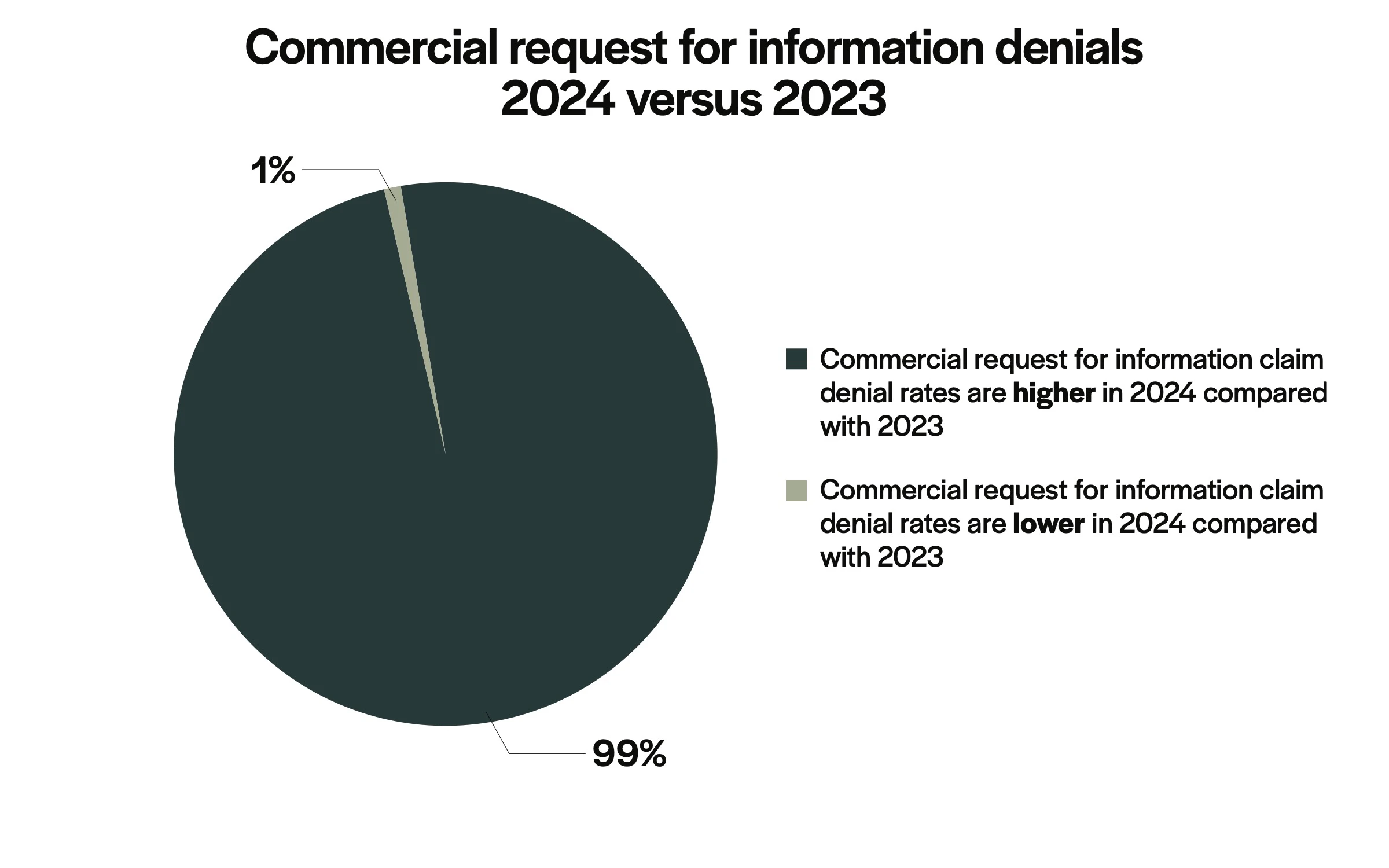
4. We asked you whether you thought request for information claim denial rates from commercial health plans are higher this year compared with 2023.
You said yes, overwhelmingly.
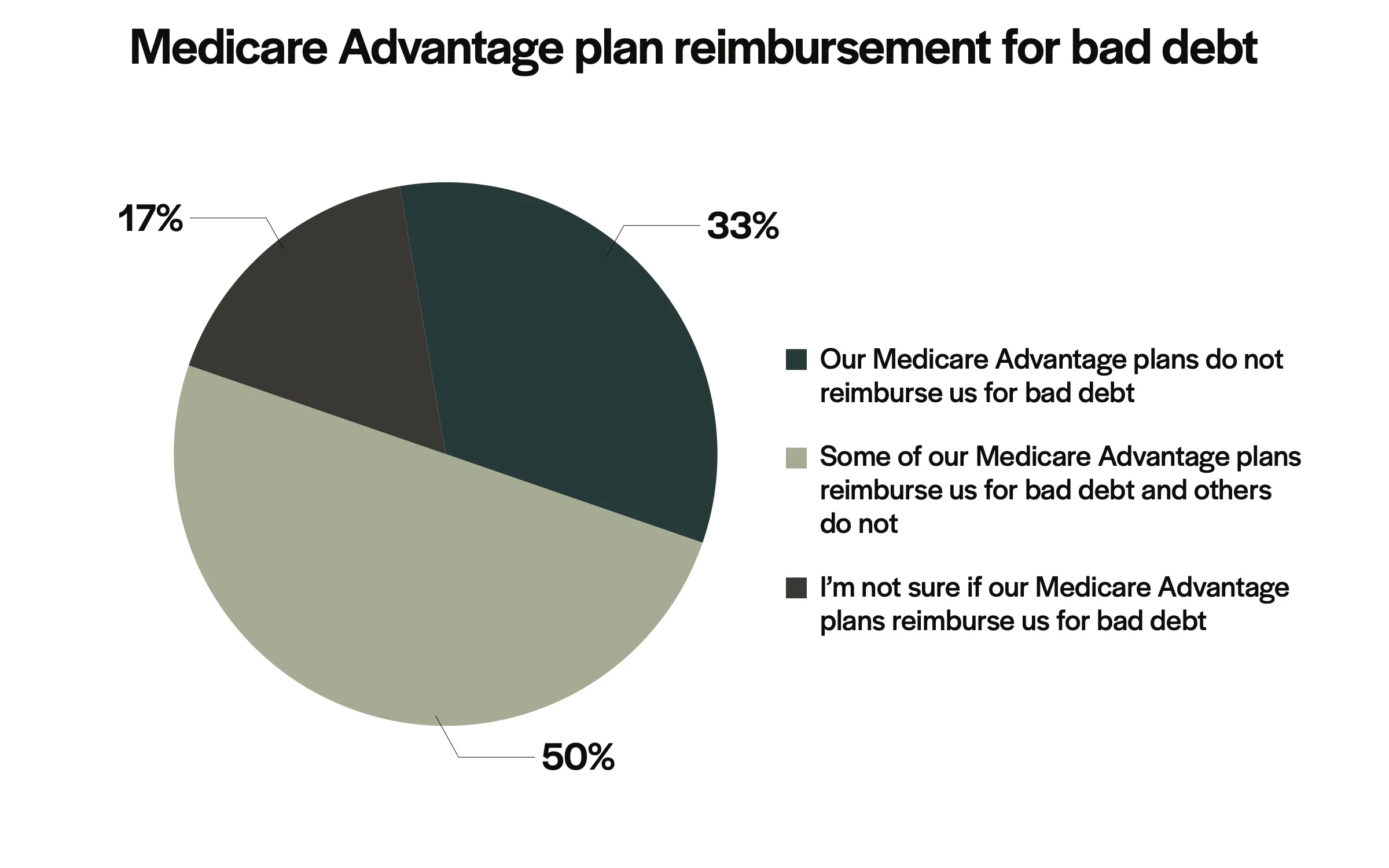
5. We asked you whether you thought your Medicare Advantage plans reimbursed you for bad debt.
One-third of you said no.
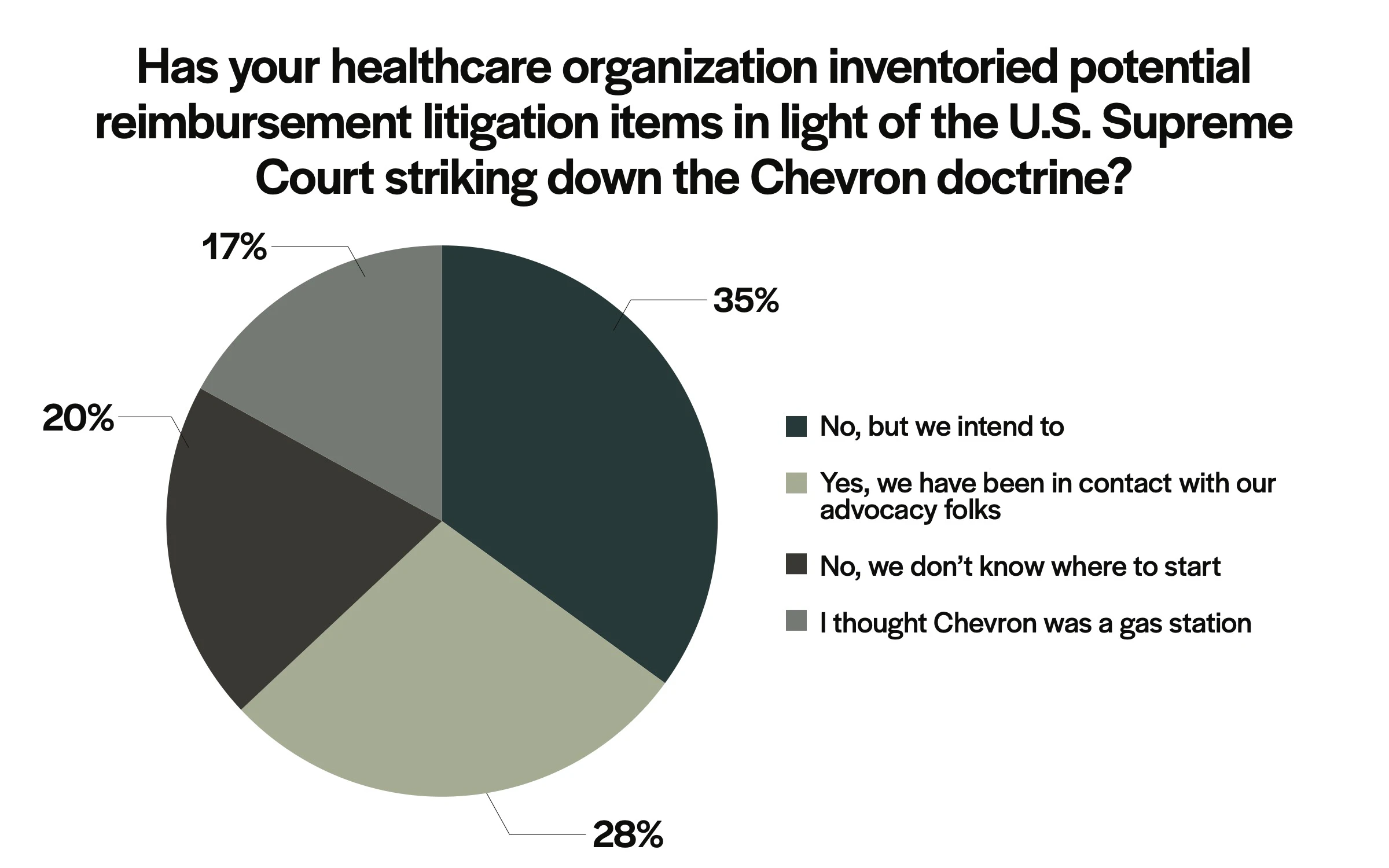
6. We asked you whether you thought your healthcare organization will inventory potential reimbursement litigation items in light of the U.S. Supreme Court striking down the Chevron doctrine and giving federal courts the power to interpret Medicare and Medicaid laws.
You said you’re definitely going to look into it.
What’s interesting about what you told us, particularly on the first four questions, is that it tracks with what we see in revenue cycle KPIs generated by Payor Market Intelligence. PMI is based on data from Kodiak Revenue Cycle Analytics, which more than 1,900 hospitals and 250,000 physicians use to manage their net revenue and monitor their revenue cycle performance.
When we normalize the KPIs, we’re seeing what you’re experiencing: more initial claim denials, higher administrative burdens and costs, significantly higher Medicare Advantage observation rates compared with traditional Medicare, and a dramatic rise in request for information denials from commercial payors.
Perception is reality.
For recommendations on how to deal with many of the issues you’ve surfaced in the Healthcare Summit attendee polls, subscribe to our monthly executive market updates. Each monthly update gives you the latest trends on 10 critical revenue cycle KPIs that have a direct impact on your net revenue performance. Each update also gives you a “tip of the month” on how to minimize the effects of the negative trends and take advantage of the positive trends.
We thank the Healthcare Summit attendees for taking our on-site and online polls and sharing their views with their colleagues and peers.
Watch for more insights from this year’s Kodiak Healthcare Summit in upcoming editions of Healthcare Connection.
Contact Us
Want the latest updates from Kodiak?
Get access to our communications, including our Healthcare Connection newsletter, to tap into industry trends, CPE webinars, and more.